Alcoholic Liver Disease (ALD) poses a formidable threat to public health, propelled by the widespread and persistent consumption of alcohol. This multifaceted condition spans a spectrum of liver afflictions, commencing with the accumulation of fat in the liver cells, known as steatosis, and progressing to more severe stages such as hepatitis and cirrhosis. Its prevalence has surged steadily over the years, cementing its status as a global health concern of considerable magnitude.
In this comprehensive exploration, we endeavor to dissect ALD from various angles, shedding light on its etiology, repercussions, underlying mechanisms, clinical manifestations, diagnostic modalities, therapeutic interventions, predisposing factors, and preventive measures. Understanding the intricate interplay of factors contributing to ALD is imperative in formulating effective strategies for its management and prevention.
The primary instigator of ALD is the chronic and excessive consumption of alcohol, which inflicts considerable damage on the liver, impairing its vital functions over time. The pathophysiology of ALD involves a complex interplay of metabolic, oxidative, and inflammatory processes, culminating in tissue injury and dysfunction.
Symptoms of ALD may vary depending on the stage and severity of the condition, encompassing a spectrum of manifestations ranging from mild discomfort to life-threatening complications. Timely diagnosis through a combination of clinical evaluation, imaging studies, and laboratory tests is crucial for initiating appropriate therapeutic interventions and mitigating the progression of the disease.
Treatment modalities for ALD span lifestyle modifications, pharmacotherapy, and, in advanced cases, liver transplantation. However, prevention remains the cornerstone in curtailing the burden of ALD, necessitating comprehensive public health initiatives aimed at raising awareness, promoting responsible alcohol consumption, and fostering early intervention strategies. Through concerted efforts and targeted interventions, the global impact of ALD can be mitigated, safeguarding the health and well-being of individuals worldwide.
Causes of ALD:
Alcoholic Liver Disease (ALD) arises predominantly from the prolonged and excessive intake of alcohol, which places an immense burden on the liver’s metabolic machinery. Upon ingestion, alcohol undergoes metabolism chiefly within the liver. However, chronic and heavy alcohol consumption surpasses the liver’s metabolic capabilities, resulting in the accumulation of toxic metabolites that wreak havoc on liver cells and incite an inflammatory response.
The liver typically metabolizes alcohol through a series of enzymatic reactions, primarily involving alcohol dehydrogenase and acetaldehyde dehydrogenase. However, when alcohol intake surpasses a certain threshold, these enzymes become overwhelmed, leading to the accumulation of acetaldehyde, a highly reactive and toxic compound. Acetaldehyde inflicts direct damage on liver cells, impairing their structure and function. Moreover, it triggers an inflammatory cascade, attracting immune cells to the liver and exacerbating tissue injury.
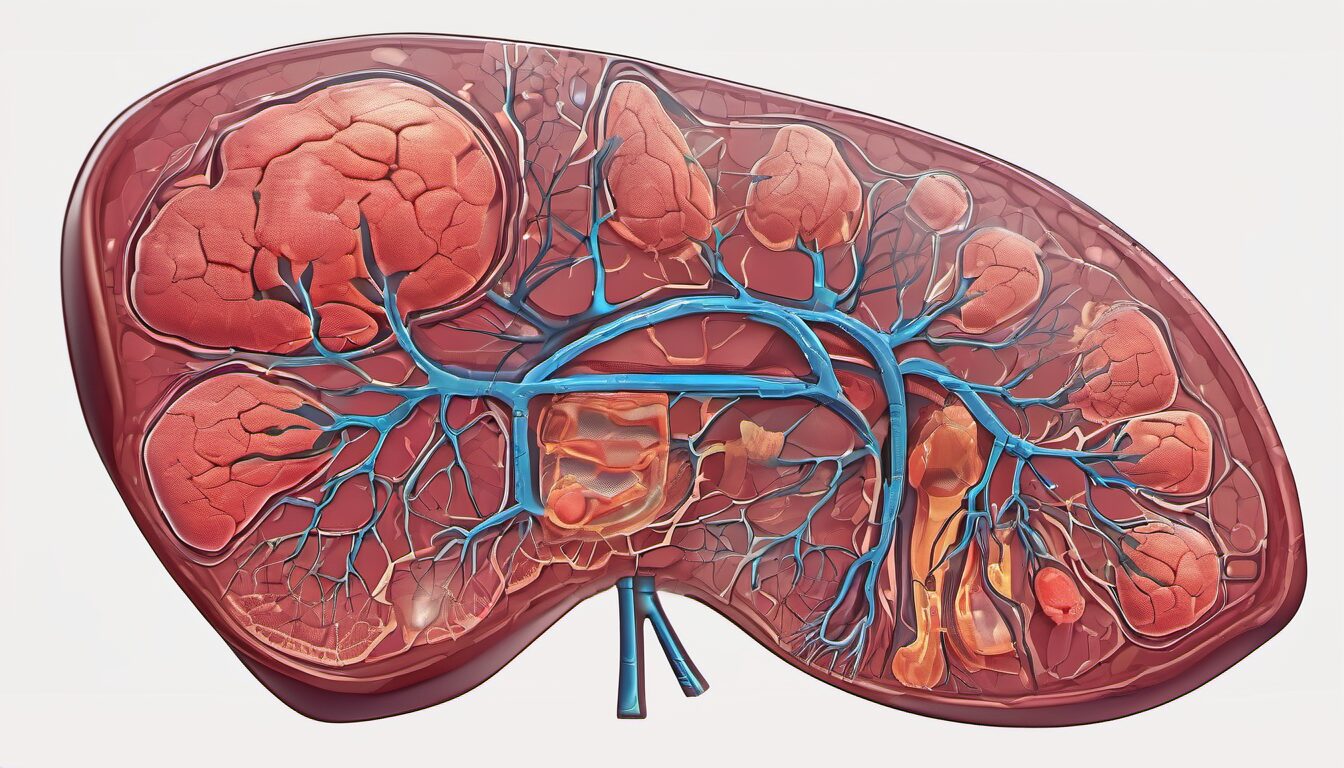
Chronic alcohol consumption also disrupts lipid metabolism within the liver, promoting the accumulation of fat droplets within hepatocytes, a condition known as steatosis or fatty liver. This lipid accumulation further compromises liver function and sets the stage for the progression of ALD to more severe forms, such as alcoholic hepatitis and cirrhosis.
Furthermore, alcohol metabolism generates oxidative stress, wherein reactive oxygen species (ROS) overwhelm the liver’s antioxidant defenses, causing oxidative damage to cellular components. This oxidative stress contributes significantly to the pathogenesis of ALD, exacerbating inflammation and accelerating liver injury.
In essence, the primary cause of ALD stems from the imbalance between alcohol intake and liver metabolism, culminating in cellular damage, inflammation, and ultimately, the progression of liver disease. Understanding these underlying mechanisms is crucial for devising effective interventions aimed at mitigating the burden of ALD and its associated complications.
The Impact of Alcohol Consumption on Liver Health:
The impact of alcohol consumption on liver health is profound and far-reaching, with even moderate drinking having deleterious effects over time. Chronic alcohol abuse disrupts numerous vital functions of the liver, compromising its ability to detoxify the body, metabolize nutrients, and synthesize essential proteins.
One of the earliest manifestations of alcohol-induced liver damage is the development of fatty liver, also known as steatosis. This condition arises due to the accumulation of fat droplets within hepatocytes, impairing liver function and setting the stage for further progression of liver disease.
Continued alcohol abuse can lead to the onset of alcoholic hepatitis, a severe and potentially life-threatening inflammation of the liver. Alcoholic hepatitis is characterized by liver cell necrosis, inflammation, and oxidative stress, culminating in liver dysfunction and potential liver failure if left unchecked.
Furthermore, prolonged alcohol exposure triggers the accumulation of scar tissue within the liver, a process known as fibrosis. Over time, this fibrotic tissue can progress to cirrhosis, a late-stage and irreversible condition marked by extensive scarring and distortion of liver architecture. Cirrhosis severely impairs liver function, leading to complications such as portal hypertension, ascites, hepatic encephalopathy, and an increased risk of liver cancer.
In summary, the impact of alcohol consumption on liver health is multifaceted and progressive, encompassing a spectrum of disorders ranging from fatty liver to cirrhosis. Recognizing the detrimental effects of alcohol on the liver underscores the importance of promoting responsible drinking behaviors and implementing interventions aimed at preventing and mitigating alcohol-related liver diseases.
Pathophysiology of ALD:
The pathophysiology of Alcoholic Liver Disease (ALD) is characterized by a cascade of intricate mechanisms orchestrated by chronic alcohol consumption. At the core of this process lies oxidative stress, provoked by the metabolism of alcohol within the liver. Alcohol metabolism generates reactive oxygen species (ROS), overwhelming the liver’s antioxidant defenses and instigating oxidative damage to cellular components.
Moreover, chronic alcohol intake elicits an inflammatory response within the liver, perpetuating tissue injury and dysfunction. This inflammation is mediated by various pro-inflammatory cytokines and immune cells recruited to the liver in response to alcohol-induced damage.
A pivotal player in ALD pathogenesis is acetaldehyde, a toxic byproduct of alcohol metabolism. Acetaldehyde inflicts direct harm on hepatocytes, disrupting cellular function and integrity. Furthermore, it contributes to oxidative stress and exacerbates inflammation, amplifying liver injury.
Persistent inflammation and hepatocyte injury stimulate the activation of fibrogenic cells, primarily hepatic stellate cells, leading to the excessive deposition of extracellular matrix proteins such as collagen. This process, known as fibrogenesis, results in the formation of scar tissue within the liver, a condition termed fibrosis.
If alcohol consumption persists unabated, the relentless cycle of inflammation, oxidative stress, and fibrosis culminates in the progression to cirrhosis. Cirrhosis represents the advanced stage of ALD, characterized by extensive liver scarring, distortion of liver architecture, and irreversible liver dysfunction.
The pathophysiology of ALD is a complex interplay of oxidative stress, inflammation, cellular injury, and fibrogenesis, ultimately leading to progressive liver damage and the development of cirrhosis in susceptible individuals with chronic alcohol abuse. Understanding these underlying mechanisms is crucial for developing targeted therapeutic strategies aimed at halting or reversing the progression of ALD and mitigating its devastating consequences.
Symptoms of ALD:
Symptoms of Alcoholic Liver Disease (ALD) manifest in a spectrum of severity, contingent upon the stage of the disease. During its initial phases, ALD may often exhibit subtle or nonspecific symptoms, making early detection challenging. Individuals may experience fatigue, vague abdominal discomfort, and unexplained weight loss, which may be overlooked or attributed to other factors.
As ALD advances, symptoms become more pronounced and indicative of significant liver dysfunction. Jaundice, characterized by the yellowing of the skin and eyes due to elevated bilirubin levels, is a hallmark manifestation of advanced liver disease. This occurs as impaired liver function hampers the processing of bilirubin, leading to its accumulation in the bloodstream and subsequent deposition in tissues.
Abdominal swelling, known as ascites, arises due to the accumulation of fluid within the abdominal cavity. Ascites develops secondary to portal hypertension, a consequence of liver fibrosis and cirrhosis, which impedes blood flow through the liver and causes fluid to accumulate in the abdomen.
Easy bruising and prolonged bleeding may occur as ALD compromises the liver’s synthesis of clotting factors, predisposing individuals to coagulopathy and spontaneous bruising or bleeding episodes.
Furthermore, ALD can manifest with cognitive impairment and altered mental status, a condition referred to as hepatic encephalopathy. Accumulation of toxins in the bloodstream, particularly ammonia, leads to neurocognitive dysfunction, resulting in confusion, disorientation, and impaired concentration.
Tthe symptoms of ALD evolve with disease progression, ranging from nonspecific manifestations such as fatigue and abdominal discomfort to more overt signs including jaundice, ascites, easy bruising, and hepatic encephalopathy. Recognizing these symptoms is crucial for prompt diagnosis and initiation of appropriate management strategies to mitigate the progression of ALD and improve patient outcomes.
Risk Factors for Disease Progression:
The progression of Alcoholic Liver Disease (ALD) from its early stages to advanced forms, including cirrhosis, is influenced by a multitude of risk factors. Understanding these factors is crucial for identifying individuals at heightened risk and implementing targeted interventions to mitigate disease progression.
Continued alcohol consumption stands as the foremost risk factor for the advancement of ALD. Prolonged and excessive alcohol intake overwhelms the liver’s metabolic capacity, exacerbating liver damage and accelerating disease progression.
Genetic predisposition also plays a significant role in ALD progression. Certain genetic variations can increase susceptibility to alcohol-induced liver injury, influencing the severity and rate of disease progression in affected individuals.
Co-existing liver conditions, such as viral hepatitis (particularly hepatitis C), synergistically potentiate the deleterious effects of alcohol on liver health. Chronic viral hepatitis exacerbates liver inflammation and fibrosis, hastening the progression to advanced stages of ALD.
Obesity and metabolic syndrome are additional risk factors that exacerbate liver damage in individuals with ALD. Obesity contributes to hepatic steatosis (fatty liver) and insulin resistance, creating a favorable environment for the progression of liver disease.
Malnutrition, commonly observed in individuals with chronic alcohol abuse, further exacerbates liver injury and impairs liver regeneration, predisposing to the development of advanced ALD.
Gender also influences the risk of ALD progression, with women generally exhibiting heightened susceptibility to alcohol-related liver damage compared to men. Physiological differences in alcohol metabolism and hormonal factors contribute to this gender disparity in ALD susceptibility.
A multitude of factors, including continued alcohol consumption, genetic predisposition, co-existing liver conditions, obesity, malnutrition, and gender, contribute to the progression of ALD to advanced stages or cirrhosis. Recognizing and addressing these risk factors are paramount in the management and prevention of ALD-associated complications, emphasizing the importance of comprehensive risk stratification and tailored intervention strategies.
Diagnosis and Treatment:
The diagnosis and treatment of Alcoholic Liver Disease (ALD) necessitate a comprehensive approach encompassing various modalities to effectively manage the condition and its associated complications.
Diagnosing ALD begins with a thorough medical history review and physical examination to assess for signs and symptoms indicative of liver dysfunction. Laboratory tests play a pivotal role in the diagnostic process, encompassing liver function tests (such as serum transaminases, bilirubin, and alkaline phosphatase levels), markers of alcohol consumption (e.g., gamma-glutamyl transferase), and evaluation for co-existing liver conditions (such as viral hepatitis).
Imaging studies, including ultrasound or computed tomography (CT) scan, provide valuable insights into liver morphology and help detect features suggestive of ALD, such as fatty infiltration or liver cirrhosis. In cases where the diagnosis remains uncertain or further characterization of liver pathology is warranted, liver biopsy may be performed to assess the extent of liver damage and guide therapeutic decisions.
Treatment strategies for ALD are multifaceted, aiming to halt disease progression, manage complications, and promote liver regeneration. Central to ALD management is the cessation of alcohol consumption, which is paramount in preventing further liver damage and halting disease progression. Nutritional support is also integral, addressing malnutrition commonly observed in individuals with ALD and facilitating liver regeneration.
Pharmacotherapy plays a pivotal role in ALD management, with medications aimed at reducing inflammation (e.g., corticosteroids), addressing oxidative stress (e.g., antioxidants), and attenuating fibrosis (e.g., pentoxifylline). In severe cases of ALD, where liver function is significantly compromised and complications are profound, liver transplantation may be considered as a definitive treatment option.
The diagnosis of ALD entails a comprehensive evaluation encompassing medical history, physical examination, laboratory tests, imaging studies, and liver biopsy. Treatment strategies for ALD focus on alcohol cessation, nutritional support, pharmacotherapy, and, in select cases, liver transplantation, with the overarching goal of halting disease progression and improving patient outcomes. Early diagnosis and prompt initiation of appropriate interventions are essential in optimizing the management of ALD and mitigating its associated morbidity and mortality.
Strategies for Prevention and Management:
Strategies for the prevention and management of Alcoholic Liver Disease (ALD) revolve around mitigating alcohol-related liver damage, adopting a healthy lifestyle, and implementing timely interventions to halt disease progression.
Preventing ALD begins with moderating alcohol consumption or abstaining from alcohol altogether. Educating individuals about the risks of excessive alcohol intake and promoting responsible drinking behaviors are paramount in reducing the incidence of ALD. For those diagnosed with ALD, cessation of alcohol consumption is imperative to prevent further liver damage and improve long-term prognosis.
In addition to alcohol cessation, adopting a healthy lifestyle plays a pivotal role in managing ALD and supporting liver health. This includes adhering to a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, while minimizing intake of processed foods, saturated fats, and added sugars. Regular physical exercise aids in weight management, improves insulin sensitivity, and enhances overall liver function.
Furthermore, avoiding other liver toxins, such as certain medications, illicit drugs, and environmental toxins, can help mitigate additional stress on the liver and reduce the risk of disease progression.
Early detection and intervention are critical in managing ALD effectively. Routine medical check-ups, including liver function tests and imaging studies, facilitate early identification of liver damage, allowing for timely implementation of therapeutic interventions. Pharmacotherapy targeting inflammation, fibrosis, and oxidative stress may be employed to halt disease progression and alleviate symptoms in individuals with ALD.
Strategies for the prevention and management of ALD encompass moderating alcohol consumption, adopting a healthy lifestyle, avoiding liver toxins, and implementing early detection and intervention measures. By emphasizing these preventive and therapeutic approaches, individuals can mitigate the risk of ALD development and improve outcomes for those affected by the disease.
In conclusion, ALD is a significant health burden associated with chronic alcohol abuse. Understanding its causes, impact, pathophysiology, symptoms, diagnosis, treatment, risk factors, and prevention strategies are essential in combating this disease. By promoting awareness, encouraging responsible alcohol consumption, and providing adequate support and treatment options, we can mitigate the detrimental effects of ALD on individuals and communities worldwide.
Disclaimer:
The information provided in this article is for informational purposes only and is not intended as medical advice. It is not a substitute for professional medical diagnosis, treatment, or advice. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment plan.









More Stories
Inside the Hormonal Symphony: Understanding the Endocrine System
Understanding Gallstones: Causes, Symptoms, and Treatment Options
The Intricacies of Cells: Exploring the Building Blocks of Life